Managing AS with Functional Medicine & Nutrition
Ankylosing Spondylitis (AS) is an autoimmune condition and inflammatory disease, which over time causes the bones in the spine to fuse and become rigid, known as Ankylosis.
AS is a form of Arthritis that affects the spine, lower back and sacroiliac joints (joints connecting the pelvic and lower spine). With this condition, the spine becomes less and less flexible, resulting in a hunched posture in some cases. If the ribs become affected by the condition, breathing deeply may become an issue.
What are the first symptoms of Ankylosing Spondylitis?
The initial symptoms of Ankylosing Spondylitis tend to be stiffness causing pain around the back, neck or hips, especially after being at rest. Fatigue is also a common first symptom for AS sufferers.
Ankylosing Spondylitis generally affects 4 areas of the body
Ankylosing spondylitis mostly affects the spine, due to the vertebrae of your spine becoming inflamed and can ultimately become calcified and fuse together. This causes back pain and stiffness. Movements such as twisting or turning of the spine can be difficult or even impossible for those living with AS. Often a hunched appearance will develop where the person stands with a stoop and cannot straighten the spine.
AS can affect other joints such as shoulders and knees, and in some cases, it can damage the eyes, heart, or lungs. AS is also associated with conditions of the skin such as psoriatic arthritis (a skin condition resulting in dry or flaky skin).
How does the Surrey Centre for Nutrition test for Ankylosing Spondylitis, using Functional Medicine?
There is not one specific test for Ankylosing Spondylitis, however there are some areas of testing which can help to determine the likelihood of AS alongside the presentation of symptoms. Most of these tests will have been done by a client's GP or consultant prior to them seeking health from the Surrey Centre for Nutrition.
Inflammatory markers may be assessed, which are often raised in those with AS, however they are not AS specific so other tests will have to take place. Testing for HLAB27 can help to narrow down the likelihood of your symptoms being caused by AS, but again this test is not diagnostic as people without AS may also have the HLAB27 gene. X ray and MRI may also be used to image the joints and tissues commonly affected by AS to determine the level of tissue destruction and degeneration.
We may at the centre also look to test gut function, intestinal permeability, food, chemical and pathogen reactivity which may help to determine some of the underlying causative factors in the development and maintenance of the disease state.
At the Surrey Centre for Nutrition we are not a diagnostic facility and therefore we are not testing to diagnose a condition or disease but with appropriate nutritional and functional testing we are able to identify triggering factors. Often we may look at running the Cyrex Array 5 panel to check if there are antibodies to any other tissue proteins. We do this to pre-empt the onset of other autoimmunities.
What is the Functional Medicine approach to Ankylosing Spondylitis, once a diagnosis is given?
Conventionally, pain medication or pain relievers are prescribed to allow the patient to take part in movement or exercise activities. Often a patient with AS will be referred to a pain clinic for medical management of pain. A physical therapist will be able to curate a program to ensure that posture and motion in the joints are kept to a good standard.
Frequently used conventional medications for AS include;
Corticosteroids
Non Steroidal Anti-Inflammatories (NSAIDs)
Immunosuppressants
Biologics
However, at the Surrey Centre for Nutrition, we opt for a more natural approach, combining Nutritional Therapy with Functional Medicine. We believe that there is not a ‘one size fits all’ treatment for any condition, therefore we conduct tests to check the underlying biochemical and physiological imbalances in the body, to be able to fully assess any underlying causative factors in a client's AS manifestation. This will aid us to provide personalised treatment and an individualised approach that suits you and your symptoms.
We often work with AS clients from a perspective of balancing gastrointestinal health, through assessment and stool testing. If we identify pathogens which may be contributing to the disease state we may target these with antimicrobials, we may also apply some probiotic therapies, and will look to support the healing and health of the mucosal lining of the gut with specific nutritional interventions. The health of the gut is so fundamentally important to inflammatory and autoimmune disease conditions that it is often the first target when we work with a person who has AS.
A client’s diet will be extensively examined, some areas we will look at include;
- intake of certain inflammatory foods and drinks such as sugar, refined carbohydrates, processed and ultra processed foods, trans fats and seed oils to name a few
- sufficiency of anti-inflammatory foods
- sufficiency of healthy fats and proteins
- nutrient density of the diet
- fibre intake
- water intake
We will then often move on to look at food reactivity, and then to investigating the chemical and pathogenic factors which may be triggering the disease state or mediating the client in that state of health.
All this said it is absolutely key that we also focus on the basics of sleep, stress, exercise in order to build a robust and well rounded protocol which targets all areas of imbalance in a client’s life, environment and diet.
However, as mentioned, every individual's case is unique, so treatment will differ from person to person with a plan created to suit your needs.
Are there any particular nutrients that can aid AS symptoms?
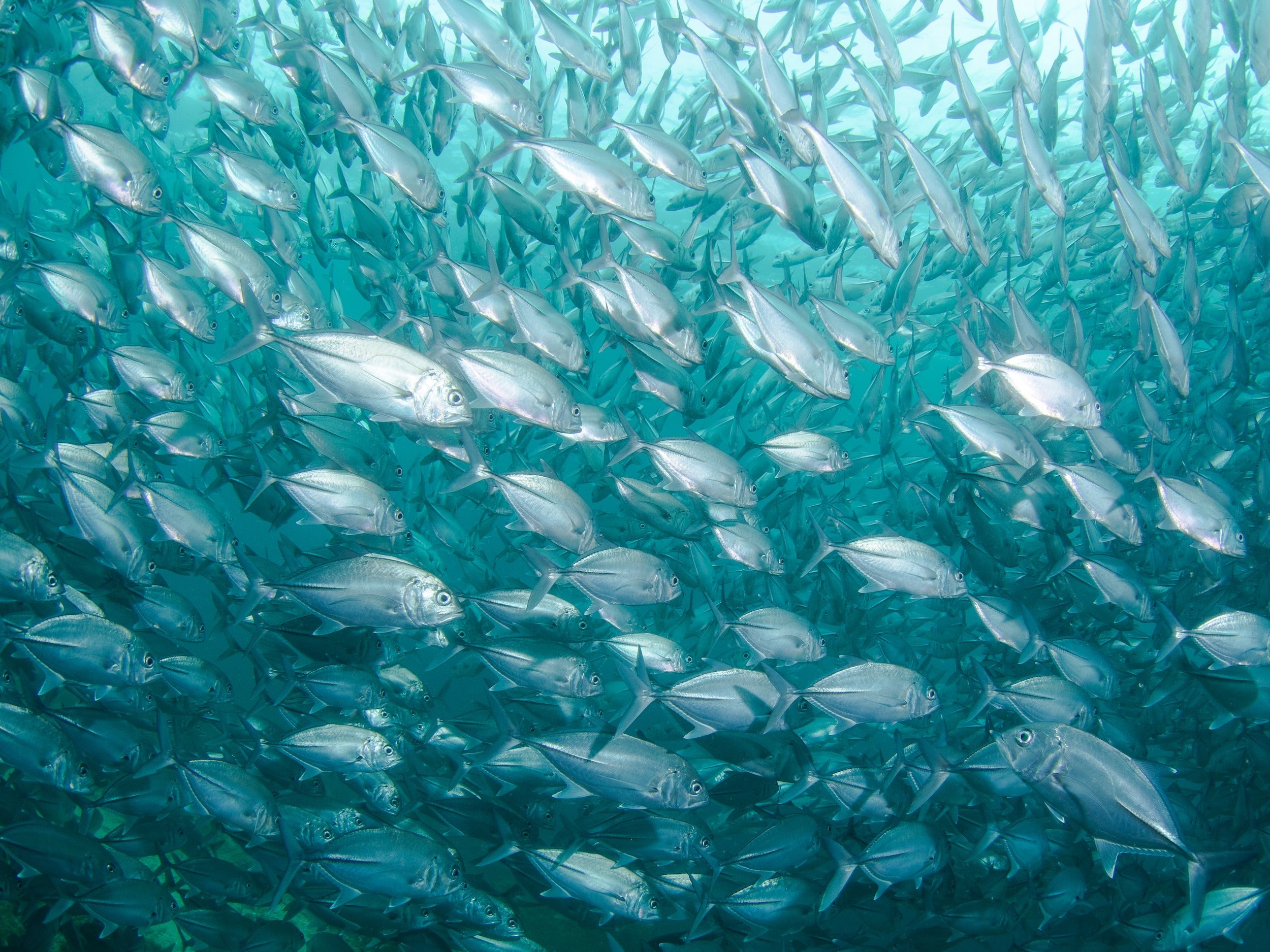
As the condition is so individualised, there is no one size fits all approach for supplementing when you have AS. Typically, immunomodulatory nutrients such as vitamin D3 are helpful, along with anti-inflammatory nutrients which we find in our vegetables, fruit, herbs and spices and essential fats such as the omega 3 fatty acids we find in oily fish.
How important is nutrition with Ankylosing Spondylitis? Are there any foods that should be avoided?
Nutrition is important when working with Ankylosing Spondylitis, therefore there are a variety of foods that should be avoided, these include:
Sugar
Refined carbohydrates
Wheat and other grains containing gluten
Dairy
Alcohol
Inflammatory seed oils
Trans fats from processed and fried foods
What should I eat if I have ankylosing spondylitis?
A basic dietary protocol for someone with AS would be a wholefoods diet, consisting of a vast array of vegetable and fruit, berries, nuts, seeds, wholegrains, legumes, healthy fats and oils such as olive and avocado oil and saturated fats from meats, good quality protein such as grass fed and organic meats, both red and white meat, fish, both oily and white but wild caught ideally, not the farmed fish.
However, this is general healthy eating guidance and often there is a need to go a few steps further with diet and look at the reduction or removal of inflammatory foods such as gluten containing grains and dairy.
Further than this, something like the Autoimmune Paleo Diet (AIP) may be considered, which further reduces the intake of possible inflammatory foods such as legumes and nightshade vegetables. This is a very restrictive protocol which should only be undertaken with the advice and guidance of a nutrition professional and is often used as a means of identifying trigger foods.
This being said, even an AIP diet may still contain foods which will trigger inflammation in an individual if they are reactive to specific foods. This is where the role of food reactivity testing comes in. At the Surrey Centre for Nutrition, food reactivity testing is something that we offer. It helps us to identify food reactivities and personalise a dietary plan to suit the client.
As much as we need to think about what we are taking out of the diet it is also important to think about what we are putting in. So make sure to include a great variety of plant foods for the beneficial fibre they contain which is supportive of gastrointestinal health and the healthy bacteria that reside in the gut and play such a massive role in immune and inflammatory processes. We also need to think about the inclusion of foods which contain important antioxidants and anti-inflammatories such as brightly coloured veg and fruit, herbs and spices. Other important foods may include probiotics such as fermented foods Kimchi, sauerkraut and kombucha, kefir.
Are you struggling with symptoms of Ankylosing Spondylitis?
Book a FREE discovery call with us at the Surrey Centre for Nutrition to opt for a natural and holistic approach to your condition. We integrate Nutritional Therapy with Functional Medicine to ensure that you have a treatment plan completely suited to you and your needs.